Team Members | Ongoing Studies | Publications | Resources | Global Knowledge Exchange Network | IPV BI Virtual Conference
3rd Intimate Partner Violence Brain Injury Virtual Conference 
5-6 November, 2025
The ENIGMA IPV Working Group and Pink Concussions are excited to announce their third 2025 ENIGMA IPV and PINK Concussions conference "Empowering Innovation: Highlighting Promising Practices in Intimate Partner Violence and Brain Injury Research, Recognition, and Response" happening November 5-6, 2025. This conference will be FREE and VIRTUAL.
REGISTRATION IS OPEN! To register, click here.
Presentations will be recorded and uploaded on ENIGMA's YouTube channel post-conference with presenters' permission.
More details here: http://esopenkolab.com/ and on the ENIGMA IPV Working Group page.


2nd Intimate Partner Violence Brain Injury Virtual Conference 
13-14 November, 2024
The ENIGMA IPV Working Group and Pink Concussions are excited to announce their second 2024 ENIGMA IPV and PINK Concussions conference "Intimate Partner Violence and Brain Injury: Breaking Down Barriers and Building Understanding" happening November 13-14, 2024. This conference will be FREE and VIRTUAL.
Based on attendee's feedback from last year, we have made some improvements to make this year's conference even more engaging and informative. Our goal is to further foster global collaboration by breaking down silos and encouraging discussions across practice, advocacy, and research. This year's conference will feature:
- Practice and advocacy-based talks aimed at improving care and services for IPV-related brain injury.
- Research-based talks focused on improving knowledge about IPV-related brain injury.
- Survivor-based sessions, providing powerful insights through personal experiences and highlighting the real-world impact of IPV-related brain injuries.
Recordings:
- Access conference recordings here. All presentations were recorded and uploaded on ENIGMA's YouTube channel with presenters' permission.
- Access conference recordings here. All presentations were recorded and uploaded on ENIGMA's YouTube channel with presenters' permission.
- Carrie Esopenko, PhD (Icahn School of Medicine at Mount Sinai)
- Kathy Chiou, PhD (University of Nebraska)
- Rachel Ramirez, LISW (Ohio DV Network)
- Elisabeth Wilde, PhD (University of Utah)
- Kathleen Monahan, DSW, LCSW (Stony Brook University)
- Kelly Russell, PhD (University of Manitoba)
- Katie Dorman, MA (Icahn School of Medicine at Mount Sinai)
- Divya Jain, PhD (Icahn School of Medicine at Mount Sinai)
- Kerri Walker (CACTIS Foundation)
- Cheryl Wellington, PhD (University of British Columbia)
More details here: http://esopenkolab.com/ and on the ENIGMA IPV Working Group page.


Speakers:


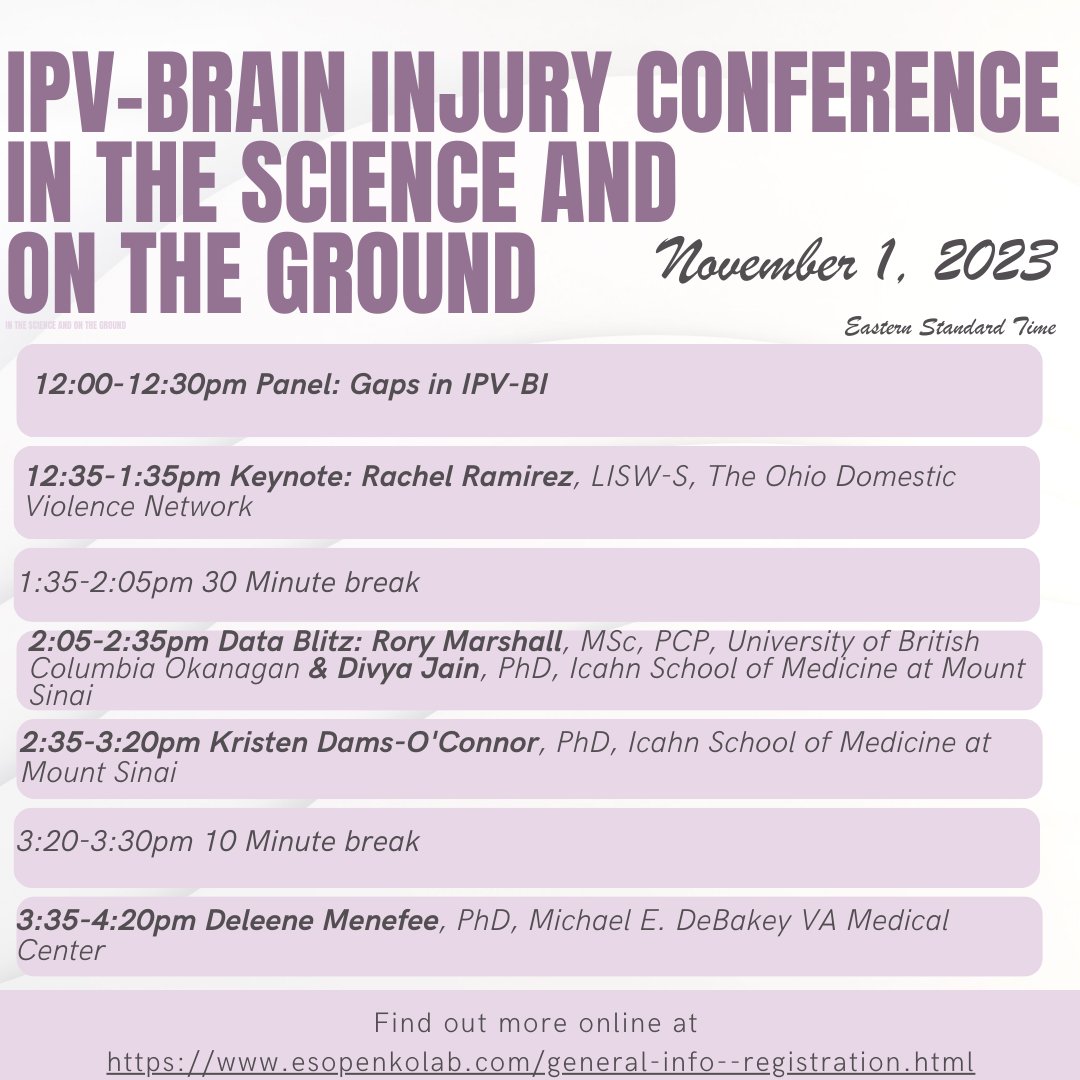
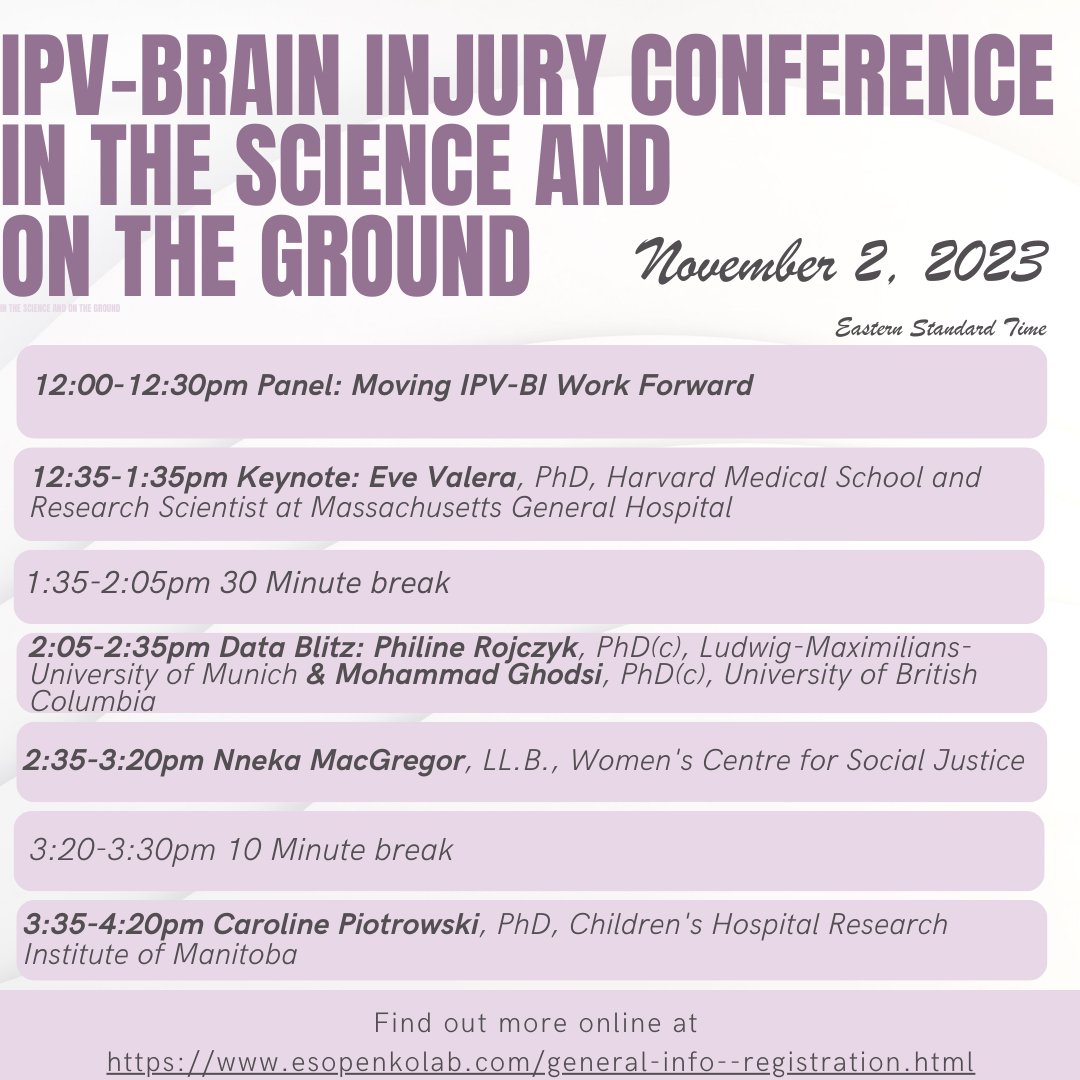
1st Intimate Partner Violence Brain Injury Virtual Conference
1-2 November, 2023
The ENIGMA IPV Working Group and Pink Concussions held their first virtual conference, Intimate Partner Violence (IPV) Brain Injury (BI) Virtual Conference: In The Science And On The Ground, on November 1-2, 2023. This conference was open and free to all, and reached over 440 individuals registrations across the globe.
More details here: http://esopenkolab.com/.
Program:
Recordings:
Organizing Committee:
Speakers:
Research and Pratice-Based Talks |
|||
|---|---|---|---|
 |
Rachel Ramirez, LISW-S (The Ohio Domestic Violence Network (ODVN)). Rachel Ramirez is the Director of Health and Disability Programs and the Founder of The Center on Partner-Inflicted Brain Injury at The Ohio Domestic Violence Network (ODVN). She provides extensive national and international training, consultation, and program support, in addition to implementing statewide projects on health access, mobile advocacy, and brain injury aware, trauma-informed and culturally responsive services. , Rachel has co-authored several peer reviewed journal articles and her work has been featured on National Public Radio as well as in The New York Times Magazine and The Washington Post. Rachel is a licensed independent social worker and a registered advocate with senior standing in Ohio and has been with ODVN for 16 years. | ||
 |
Eve Valera, PhD (Harvard Medical School/Massachusetts General Hospital). Dr. Eve Valera, Associate Professor in Psychiatry at Harvard Medical School and Research Scientist at Massachusetts General Hospital has worked in the domestic violence field for over 25 years. She uses a range of methodologies to understand the neural, cognitive and psychological consequences of brain injuries from intimate-partner violence, with her most recent focus being on transgender women. As a pioneer in the field of IPV-related brain injury, she regularly lectures internationally and has received national and international recognition for her work being featured in news outlets such as NYT Magazine and Forbes. She was an inaugural recipient of the Women Making History Award from Safe Living Spaces and has also been the recipient of the prestigious Robert D. Voogt Founders Award, Rappaport Research Fellowship in Neurology, PINK Concussions Domestic Violence Award and the Anne Klibanski Visiting Scholars Award. She is passionate about raising awareness and educating all relevant stakeholders about this tremendously overlooked public health problem. | ||
Research and Pratice-Based Talks |
|||
|---|---|---|---|
 |
Kristen Dams-O'Connor, PhD (Icahn School of Medicine at Mount Sinai Hospital). Dr. Kristen Dams-O'Connor is Director of the Brain Injury Research Center of Mount Sinai, a clinical neuropsychologist, Jack Nash Professor in the Departments of Rehabilitation Medicine and Neurology at Icahn School of Medicine at Mount Sinai, and the Project Director of the New York Traumatic Brain Injury Model System of Care. She completed a postdoctoral fellowship in clinical neuropsychology at Mount Sinai Medical Center, and a predoctoral internship in neurorehabilitation at the Rusk Institute of Rehabilitation Medicine at New York University Medical Center. She received her Ph.D. from the University at Albany. She has published over 150 peer-reviewed manuscripts and chapters on traumatic brain injury treatments and outcomes, and has presented her research internationally. Her primary fields of clinical and research expertise are in long-term outcomes after brain injury, intersections of TBI and neurodegenerative disease, neuropsychological assessment, and cognitive rehabilitation for individuals with neurological diseases. Her research is currently supported by federal grants from the National Institutes of Health, National Institute for Disability and Rehabilitation Research, and the Department of Defense. | ||
 |
Nneka MacGregor, LL.B. (Women's Centre for Social Justice). Nneka MacGregor, LL.B. is co-founder and Executive Director of the Women's Centre for Social Justice, better known as WomenatthecentrE, a unique non-profit created by and for women, trans and gender-diverse survivors of gender-based violence (GBV). A Black intersectional abolitionist feminist, international speaker & trainer, she is an expert advisory panel member of the Canadian Femicide Observatory for Justice and Accountability and sits on several advisory Boards and committees, including the Federal Advisory Council on the Federal Strategy Against GBV, and co-founded the Black Femicide Canada Council. Her research focuses on Black femicide, sexual violence, and the intersection of strangulation, Traumatic Brain Injury, and Inter-personal violence. She received the 2019 PINK Concussions Award and the 2020 YWCA Toronto Women of Distinction Social Justice Award. She is founder and Managing Partner of Nneka & Co, a consulting firm of BIPOC activists that focuses on Stakeholder-Centric EDI© - a unique and comprehensive framework to engage organisations in equity, diversity & inclusion work. Her expertise is on nurturing women’s leadership in business at the intersection of gender, race, and ability. Nneka was a member of the Board of Directors of Moatfield Foundation of Bayview Glen School, where she served as Chair and Board President for six years. She supports other charitable and non-profit organisations with governance training and developing effective Board culture. | ||
 |
Deleene Menefee, PhD (Baylor College of Medicine). Dr. Deleene Menefee obtained her graduate psychology degree from the University of Houston and completed predoctoral internship at the Michael E. DeBakey VA Medical Center. She joined the faculty at MEDVAMC in August of 2008, after completing a postdoctoral fellowship in serious mental illness. Dr. Menefee is a practicing Texas licensed psychologist and currently the Women Veterans Program Manager at the Houston VA. She has extensive experience providing trauma-informed mental health services to veterans of all eras but has a strong passion for equitable services for women Veterans. In addition to her academic appointment as an assistant professor at Baylor College of Medicine, Dr. Menefee also serves as the Houston site lead for the Women’s Health Practice Based Research Network. Her areas of research include PTSD from military-related trauma and interpersonal violence, examining reintegration issues with returning veterans, trauma-informed treatment, and treatment outcomes that inform best practices for the unique mental health needs of women veterans. | ||
 |
Caroline Piotrowski, PhD (Children's Hospital Research Institute of Manitoba). Dr. Caroline Piotrowski is an Associate Professor in the Department of Community Health Sciences and a Scientist at Children's Hospital Research Institute of Manitoba. Her background includes developmental psychology, lifespan human development, and health promotion. Her areas of expertise include the effects of exposure to intimate partner violence on children, trauma and resilience in young people and their families, posttraumatic growth, and sibling relationships. She is particularly interested in how the social determinants of health interact with family factors to influence risk and protective factors for violence and injury. She is currently leading an international multidisciplinary team evaluating an intervention for Indigenous mothers and children affected by intimate partner violence in Canada. | ||
Panels |
|||
|---|---|---|---|
 |
Kathy Chiou, PhD (University of Nebraska-Lincoln). Dr. Kathy Chiou received her Ph.D. in Psychology from the Pennsylvania State University. She completed her pre-doctoral clinical internship with an emphasis in neuropsychology at the University of Florida Health Sciences Center and her post-doctoral fellowship at the Kessler Foundation. She is currently an Assistant Professor in the department of Psychology at the University of Nebraska-Lincoln. Her program of research is aimed at understanding bio, psycho, and socio-determinants of cognitive functioning and outcome following traumatic brain injury (TBI). Dr. Chiou also has particular interests in studying TBI in vulnerable, at-risk, and underserved populations. Projects in this area aim to: 1) understand the effects of brain injury as it occurs in complex, intersecting contexts of culture, mental, and behavioral health, and 2) identify and address disparities in outcomes and access to care after injury. She hopes that research in this area will help bring about systematic changes to service delivery that ultimately improve outcomes and quality of life for survivors with brain injury. | ||
 |
Brenda Eagan-Johnson, ED (BrainSTEPS). Brenda Eagan-Johnson, EdD, CBIST-AP directs the nationally recognized brain injury school consulting program, BrainSTEPS in Pennsylvania. Her doctorate is in the neuroscience of education from Johns Hopkins University. Dr. Eagan-Johnson serves on the Board of Governors for the Academy of Certified Brain Injury Specialists under the Brain Injury Association of America and Board of Directors for the International Pediatric Brain Injury Society. She is a Certified Brain Injury Specialist Trainer with Advanced Practice in NeuroRehabilitation. Dr. Eagan-Johnson served for several years as a consultant to the Colorado Department of Education to assist their BrainSTEPS Program development and is an expert consultant for several research studies investigating brain injury. She also served several years as an instructor at George Washington University where she taught graduate-level brain injury coursework. Dr. Eagan-Johnson is published in the field of pediatric brain injury and has won multiple awards for her work. She is an active member of the ENIGMA Brain Injury IPV group and co-leads the National Association of State Head Injury Administrators Collaborative on Children's Brain Injury. Dr. Eagan-Johnson is a strong advocate for social justice and has been asked to present numerous times for national and federal organizations regarding IPV and child abuse, including a Congressional panel and Senate briefing panel in Washington, D.C. She has a sibling who sustained a severe traumatic brain injury while they were teenagers, which is where her passion for helping students, families, and schools began. | ||
 |
Halina (Lin) Haag, MSW/RSW/PhD(c) (Wilfrid Laurier University/University of Toronto). Ms Halina (Lin) Haag, MSW, RSW, PhD(c) is a PhD candidate and Contract Faculty member with the Faculty of Social Work at Wilfrid Laurier University and a research trainee at the Acquired Brain Injury Research Lab at the University of Toronto. She is exploring the gendered experiences of brain injury and the barriers and facilitating factors influencing mental health, return to work, and social integration encountered by brain injured women survivors of intimate partner violence. Lin is committed to improving outcomes through direct practice, innovative research, and professional education, believing that increased knowledge and understanding in the community is key. In 2021 she was honoured to recieve the Neurological Health Charities of Canada’s Changemaker Award for her work in IPV-related brain injury. As someone with lived experience of brain injury, she has been a guest speaker addressing issues of disability, brain injury, and marginalization for a variety of international academic, professional, and community-based organizations. Her work has been generously funded by the Ontario Women’s Health Scholar Award. | ||
 |
Katherine (Kate) Iverson, PhD (VA Boston Healthcare System/Boston University School of Medicine). Dr. Katherine (Kate) Iverson, PhD is a clinical psychologist, health services researcher, and implementation scientist who aims to improve healthcare services for individuals who experience trauma, particularly intimate partner violence (IPV). She is a Clinician Investigator in the Women’s Health Sciences Division of the National Center for PTSD at the VA Boston Healthcare System and Associate Professor of Psychiatry at Boston University School of Medicine. Dr. Iverson’s research ranges from identifying the prevalence of IPV and associated health consequences (e.g., PTSD and brain injury), to developing and evaluating treatments for individuals who experience IPV, to implementing IPV screening programs and treatments into routine care. The clinical and policy impacts for the Veterans Health Administration (VHA) were recognized through a Presidential Early Career Award for Scientists and Engineers. She has published more than 120 peer-reviewed journal articles on IPV and related topics such as brain PTSD, brain injury, and trauma-informed care. Dr. Iverson also co-developed and established the evidence-base for a holistic, trauma-informed, and patient-centered brief counseling intervention that is being rolled out in the VHA- “Recovering from IPV through Strengths and Empowerment” (RISE)- for patients who experience recent or ongoing IPV. | ||
 |
Johnny Lifshitz, PhD (Phoenix VA Health Care System/University of Arizona College of Medicine – Phoenix). Jonathan Lifshitz, PhD, leads the Neurotrauma & Social Impact research team as a joint venture between the Phoenix VA Health Care System and University of Arizona College of Medicine - Phoenix. Research investigations focus on restorative and regenerative treatments for traumatic brain injury as it develops into chronic neurodegenerative disease. We investigate domestic violence, child abuse, gender imbalance, marital norms, and Veteran mental health. The goal is to translate findings to improve the health of our communities through precision diagnostics, rehabilitation, and new knowledge. He earned a Bachelors in Neuroscience from UCLA, a PhD in Neuroscience from University of Pennsylvania, and completed fellowships at UPenn and VCU. He leads local, state, and federal funded projects, including ones on cognitive rehabilitation, cardiovascular risk factors, systemic effects of brain injury, and vital imaging. Currently, he is the scientific director for regional and national consortia to understand traumatic brain injury arising from domestic violence. He chaired the Arizona Governor’s Council on Spinal and Head Injury, co-hosts the UArizona COM-P podcast ReImagine Medicine, and is the Lead Scientist and Director of Research and Development for The CACTIS Foundation. | ||
 |
Karen Mason (Supporting Survivors of Abuse and Brain Injury through Research - SOAR). Karen Mason (she/her) is co-founder and executive director for Supporting Survivors of Abuse and Brain Injury through Research (SOAR), and former executive director of Kelowna Women’s Shelter and Third Space Charity in Kelowna, British Columbia, Canada. A seasoned non-profit leader, communicator, and community collaborator, Mason brings 30+ years of career experience in the private, public, and non-profit sectors to her work advocating for survivors of IPV, conducting knowledge translation and mobilization activities, and supporting research, development, and dissemination of promising practices. Mason has training in advanced strangulation prevention, and is a member of the Pink Concussions Partner-Inflicted Brain Injury Task Force, and the ENIGMA International Consortium Working Group on Brain Injury in Intimate Partner Violence. | ||
 |
Julianna Nemeth, PhD (The Ohio State University). Julianna M. Nemeth, PhD, MA, is an Assistant Professor of Public Health at The Ohio State University. Dr. Nemeth is a health equity intervention scientist. Her research focuses on optimizing interpersonal and structural interventions to be delivered through trusted community organizations serving populations impacted by trauma—including unstably-housed youth, gender-based violence survivors, and people living in geographic communities hardest hit by COVID-19. Dr. Nemeth focuses on identifying modifiable mechanistic targets for intervention—with the ultimate goal of increasing equitable 1) access to social determinants facilitating health and 2) success with behavioral change. I returned to graduate school in 2010 after having worked for over 10 years as a community-advocate, in court, hospital, and non-profit settings, alongside survivors of sexual and domestic violence (DV). During this time, I worked to found The Ohio Alliance to End Sexual Violence. Through the course of my formative research career, I have partnered with the Ohio Domestic Violence Network on the discovery that undiagnosed brain injury from intimate partner violence, and other forms of interpersonal violence used to maintain structural power, are pervasive among violence survivors seeking safety and other social services. Therefore, my research now focuses on increasing the capacity of organizations to identify, accommodate, and create care pathways for violence survivors living with brain injury from violence. | ||
 |
Mary Jane Pugh, PhD (George E Whalen Veteran Affairs Hospital SLC/Professor at the University of Utah). Integrating her training as a Veteran, nurse, and developmental psychologist, Dr. Mary Jane Pugh developed a research program to examine the long-term sequelae and outcomes of military exposures. Over the past decade her work has used VA data to identify phenotypes in populations with complex comorbidity including those with traumatic brain injury (TBI). Dr. Pugh’s current work includes longitudinal observational and prospective studies to identify the emergence of distinct neurodegenerative conditions such as cognitive impairment and epilepsy that may have similar/networked biological underpinnings. Her longitudinal population-based observational studies currently link Department of Defense combat theatre and health system data with VA health system data with primary data collection including survey, neuroimaging, neuropsychological testing, and biomarkers. These studies currently using health system and survey data to identify IPV across the lifespan and to identify approaches to mitigate negative outcomes. | ||
 |
Katherine Price Snedaker, LCSW (PINK Concussions). Katherine Price Snedaker, LCSW, is the pro-bono Executive Director and Founder of PINK Concussions, as well as international keynote speaker, therapist, and published researcher who has experienced brain injury in her family. Katherine founded PINK Concussions in 2012, to improve the care and recovery of women and girls by educating the public, patients and medical professionals on sex and gender differences in brain injury. Including domestic violence in the title of the NGO along with sports and military service was unheard of at the time as awareness of TBI in DV was not well known. But Katherine strongly believed that beyond sports, there was a far greater number of repetitive brain injuries are still hidden and endured by the invisible women who suffer violence inflicted by partners in every social economic group of society. Katherine has always advocated for Information on women who suffer brain injuries from violence in their homes or communities to be included in all community brain injury education, medical trainings, and any research plans. In January 2019, Katherine launched the PINK Concussions Partner-Inflicted Brain Injury Task Force to bring together brain injury experts with domestic violence/intimate partner violence professionals. This international task force lead by six experts in the field seeks to improve the lives of those impacted by violence by creating an open space for learning, inspiration, and collaboration among those working in brain injury and gender-based violence. | ||
 |
William Stewart, PhD (Queen Elizabeth University Hospital/University of Pennsylvania). Dr. William Stewart is Consultant Neuropathologist at the Queen Elizabeth University Hospital, Glasgow, and holds honorary Associate Professor status at the University of Glasgow (Institute of Neuroscience & Psychology) and the University of Pennsylvania (Department of Neurosurgery). Dr. Stewart leads an internationally regarded research laboratory engaged in multiple programs investigating the pathologies of acute and long-term survival from traumatic brain injury (TBI). Working with the unique and comprehensive Glasgow TBI Archive, Dr. Stewart’s research describes the complex neuropathology of brain injury across a range of exposures and survivals, with particular reference to the link between TBI and neurodegenerative disease. Dr. Stewart directs the FIELD study, which aims to describe lifelong health and dementia risk in former soccer, and is Co-PI on the multi-centre collaborative research program CONNECT-TBI. | ||
 |
Paul van Donkelaar, PhD (Supporting Survivors of Abuse and Brain Injury through Research - SOAR/University of British Columbia). Dr. Paul van Donkelaar (he/him) is co-founder and scientific advisory for Supporting Survivors of Abuse and Brain Injury through Research (SOAR). He is also a professor in the School of Health and Exercise Sciences and Associate Vice Principal, Research at the University of British Columbia’s Okanagan campus in Kelowna, British Columbia, Canada. His research focuses on the basic mechanisms of sensorimotor control and the cerebrovascular, neurocognitive, and sensorimotor aspects of brain dysfunction resulting from traumatic brain injury. Since 2016, he has focused the majority of his work on better understanding brain dysfunction in women who have experienced intimate partner violence-caused brain injury through the SOAR project. Dr. van Donkelaar is a member of the Pink Concussions Partner-Inflicted Brain Injury Task Force, and the ENIGMA International Consortium Working Group on Brain Injury in Intimate Partner Violence. | ||
Trainee Data Blitz |
|||
|---|---|---|---|
 |
Mohammad Ghodsi (University of British Columbia). Mohammad Ghodsi is a first-year graduate student in the Department of Pathology and Laboratory Medicine at the University of British Columbia, under the supervision of Dr. Cheryl Wellington. He is currently studying for his Master of Science degree. He is exploring how fluid-based neurological biomarkers can improve the diagnosis of brain injury due to intimate partner violence. | ||
 |
Divya Jain, PhD (Icahn School of Medicine at Mount Sinai). Dr. Divya Jain earned her PhD in bioengineering from the University of Pennsylvania and the Center for Injury Research and Prevention at the Children’s Hospital of Philadelphia, co-advised by Dr. Kristy Arbogast and Dr. Catherine McDonald. She completed her BS in bioengineering from the University of Maryland, College Park and as a result, is a die-hard Terps fan. She is now a post-doctoral fellow working with Dr. Carrie Esopenko at the Icahn School of Medicine at Mount Sinai. | ||
 |
Rory A. Marshall, MSc, PCP (University of British Columbia Okanagan). Rory A. Marshall is a PhD Candidate at the School of Health and Exercise Sciences in the Faculty of Health and Social Development at the University of British Columbia Okanagan and a paramedic working with Alberta Health Services and British Columbia Emergency Health Services, respectively. Rory earned his Bachelor’s degree in Kinesiology and Business at Vancouver Island University and his Master’s degree in Biomedical Sciences at the University of Saskatchewan. He has also had international paramedic experience practicing in New Zealand and Central America. Rory’s research interests include intimate partner violence, intimate partner violence-caused brain injury, paramedicine, and resuscitation. Rory is a Senior Fellow at the McNally Project for Paramedic Research. Rory can be reached at Rory.Marshall@ubc.ca or on Twitter @RoryAMarshall. | ||
 |
Philine Rojczyk, MSc (Ludwig-Maximilians-University of Munich). Philine Rojczyk is a Ph.D. student at Child Brain Research And Imaging in Neuroscience (cBRAIN), Ludwig-Maximilians-University of Munich, where she focuses on diffusion tensor imaging of white matter microstructural integrity in patients with mild traumatic brain injury and post-traumatic stress disorder. She was trained in psychology (B.Sc. Leiden University, The Netherlands; M.Sc. Medical School Hamburg, Germany) and specialized in clinical psychology, neuropsychology and cognitive neuroscience. During her Ph.D., she spent a one-year traineeship at the Psychiatry Neuroimaging Laboratory (PNL), Harvard Medical School where she acquired knowledge on advanced neuroimaging data processing techniques when working on a project of military war veterans with mild traumatic brain injury and post-traumatic stress disorder. Philine joined the ENIGMA IPV group in the aim of exploring brain structural alterations associated with intimate partner violence victimization and perpetration. | ||